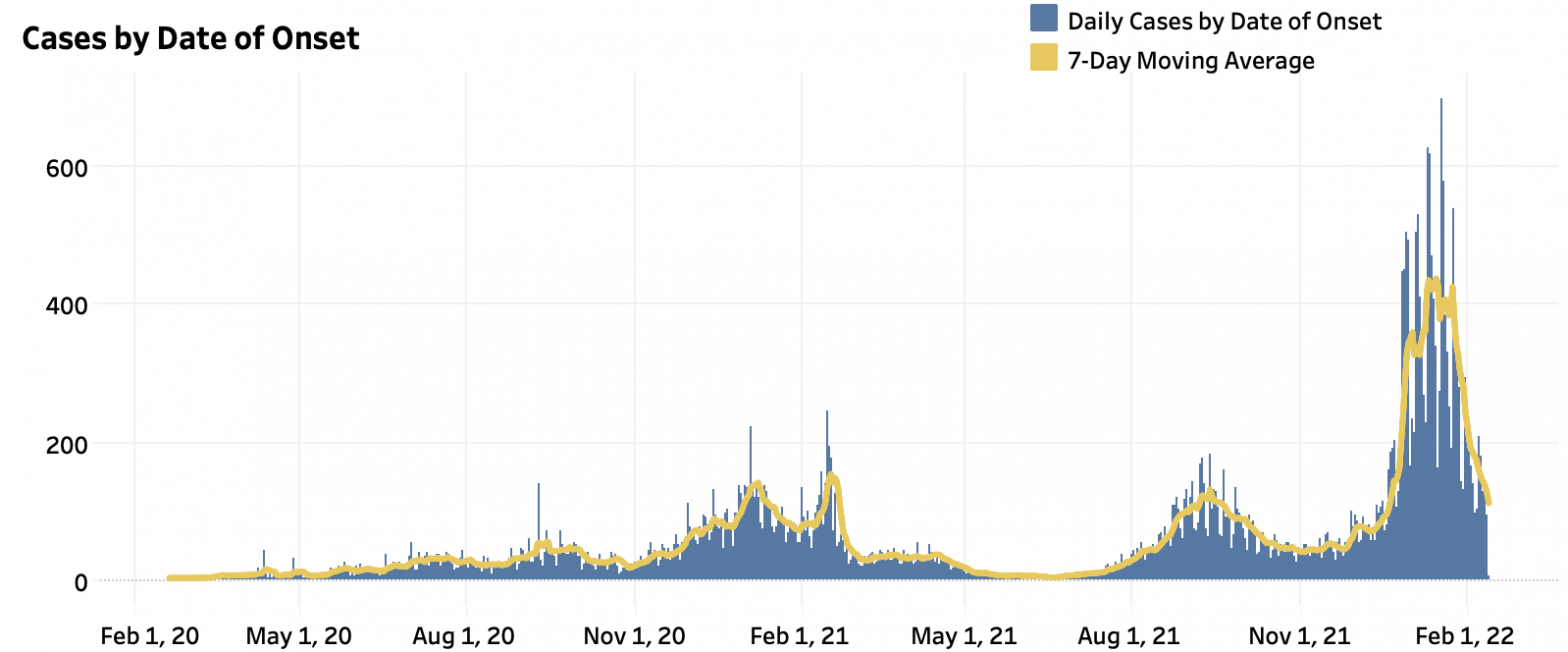
In January, the highly contagious omicron variant brought coronavirus cases to an all-time high in the Charlottesville area. The Blue Ridge Health District reported over 11,000 new cases and nearly 200 hospitalizations—the largest surge since the pandemic started in February 2020.
Over the past few weeks, cases and hospitalizations have significantly declined. On February 13, the health district reported just six new cases. However, UVA Health employees continue to reel from the surge, which heaped additional stress upon the hospital’s limited staff.
“On my days off in January, every day it seemed like I was getting a text from work, [saying] ‘hey do you want to come and pick up, because we’re running close,’” says a UVA nurse, who wishes to remain anonymous out of fear of retaliation. “It was that way all over the hospital.”
Last month, the hospital admitted over 100 coronavirus patients. Many nurses contracted the virus and had to quarantine at home, worsening the hospital’s staffing crisis.
“We started to see more patients who maybe weren’t in the hospital for COVID necessarily, but we later found out they were COVID positive,” says the nurse. “You have to put them on special isolation precautions, which makes them much more labor intensive to take care of.”
Over the course of the pandemic, intense burnout and exhaustion has led numerous health care workers to call it quits. Some units have lost all of their core staff, and are completely reliant on travel nurses, claims the nurse.
According to UVA Health spokesman Eric Swensen, about 21 percent of hospital staff—including nearly 25 percent of nurses—turned over last year. To recruit more employees, the hospital has ramped up its partnerships with nursing schools across the country, as well as developed paid training programs for various positions, like pharmacy technicians. From August to January, the hospital has hired 865 new employees.
This month, the health system received over $2 million in federal funding to expand its peer support program, designed to reduce burnout and stress, and promote mental wellness. The program, Wisdom & Wellbeing, trains employees to identify and address stressors in themselves and their co-workers, and connects them with helpful resources, including exercise classes, nutrition services, and professional counseling, explains program co-creator Dr. Richard Westphal.
“If we can recognize when we have a co-worker who has a potential stress-related illness, how do we help them get connected with professional help early?” says Westphal. “We all know that the earlier that someone engages with therapy and professional services when they have the emerging symptoms of a mental disorder, the better the outcomes.”
Though the nurse believes the wellness program is “well-intentioned,” he thinks the hospital should pay employees better. Last fall, the health system announced it planned to spend more than $30 million this fiscal year on long-awaited wage increases. He’d also like to see employees have more decision-making power.
“Make our wages competitive with travelers—that’s what would make us feel appreciated,” he says.
To keep coronavirus cases down—and reduce the heavy burden on health care workers—community members are encouraged to get vaccinated, wear N95 masks, and social distance. Immunocompromised individuals are now eligible to receive a fourth dose of the coronavirus vaccine three months after their third dose.
“If you know a health care worker, just stay in touch with them and see how they’re doing,” says the nurse.